OMNIA Q&A: The Future of COVID-19
David S. Roos, E. Otis Kendall Professor of Biology, on COVID-19, variants, and vaccines.
As information about potentially more virulent strains of COVID-19 continues to emerge, OMNIA talked with David S. Roos, E. Otis Kendall Professor of Biology, who studies and teaches infectious disease biology, viruses, and parasites. We asked him how concerned Americans should be about variants, the promise of coronavirus vaccines, the future of the virus, and the potential for another pandemic.
You’re an infectious disease biologist. Has anything about how COVID-19 behaves surprised you?
Perhaps the biggest surprise, which we still don’t understand, is why some people get very sick or die, while others don't. There are some theories about inappropriate immune responses, including so-called cytokine storms, and there's some evidence for viral engagement with other aspects of human pathology, but there’s still a lot to learn about the disease processes caused by the SARS-CoV2 virus that causes Covid-19.
How do you stay current on the latest COVID-19 data and the emerging variants?
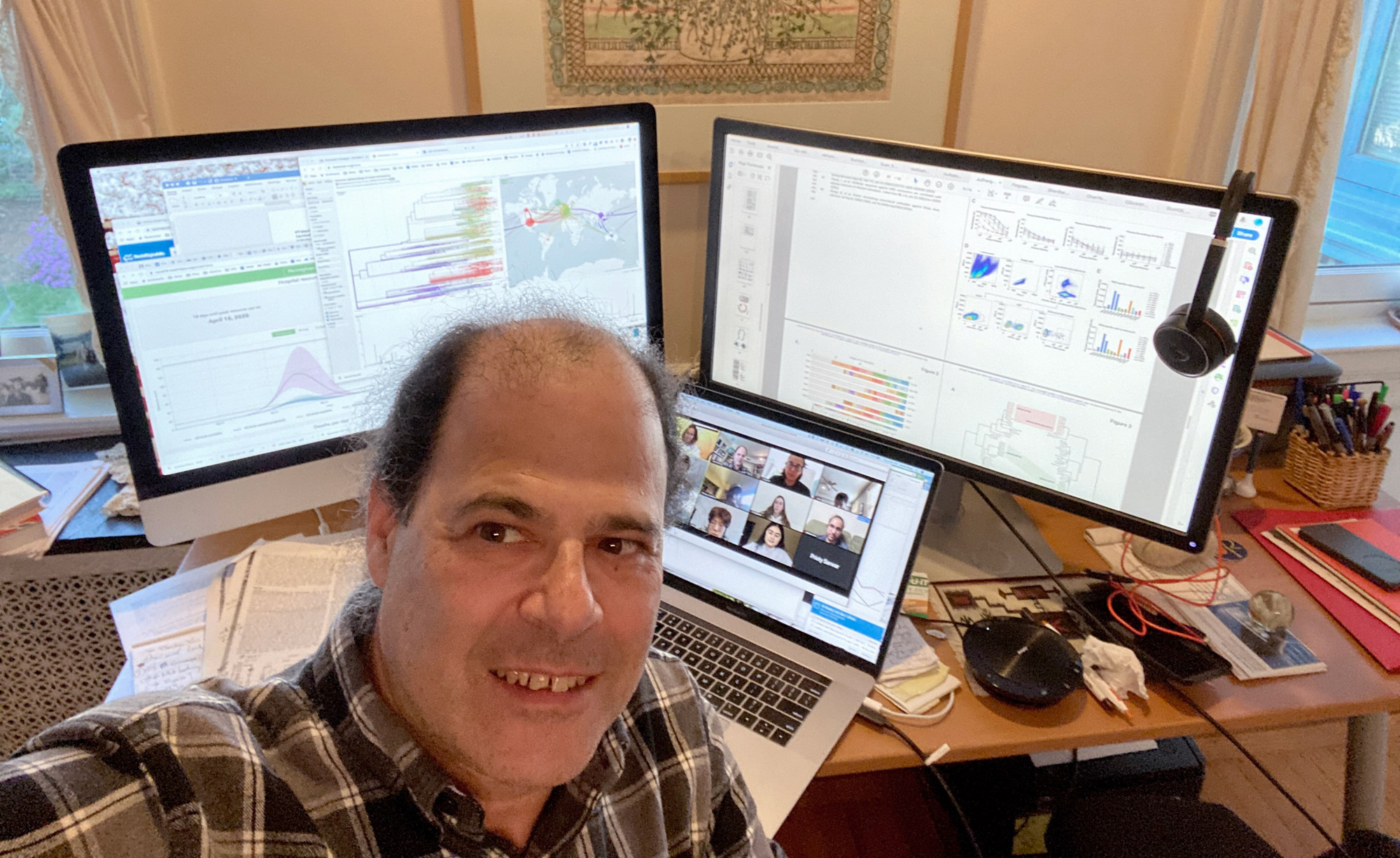
I follow quite a few web sites, as well as preprint servers that post scientific studies in advance of formal review. For example, I often use a site called NextStrain.org that tracks pathogen evolution. Using this site, you can follow the worldwide evolution of the virus in near real-time. Looking across the entire viral genome of 29,000 nucleotides, the different colored bits—green, orange, blue, etc.—represent distinct proteins. The lines extending vertically represent the frequency of various mutations identified around the world. The map lets you see where these viruses were isolated, and the evolutionary tree allows you to track how they are related. We can clearly see that the devastating outbreak in New York last spring arrived from China via Europe, and you can see that there are now numerous mutations emerging all over the world.
How concerned are you about these COVID-19 variants?
Am I inherently concerned about viral variation? Not necessarily. Nearly every virus is likely to be slightly different than its parents. The same is true for our cells. We have trillions of cells in our body, and each one is likely to have acquired minor mutations compared with its parents—typographical errors, if you will. Do you care that the DNA in one cheek cell might be slightly different than the DNA in another cheek cell? Probably not, except in the relatively rare case these mutations may allow the cell to grow uncontrollably, as a cancer.
Imagine that you are concerned that Shakespeare’s Hamlet gets passed down uncorrupted across the generations. Act I contains about as many letters as the coronavirus genome. If you had to copy that manuscript manually, you’d probably introduce a few typos. These are unlikely to significantly change the meaning of the play, but if someone else transcribes your copy, rather than going back to the original, and this process is repeated over and over, you’d ultimately wind up with rubbish. A garbled manuscript will probably be ignored, in favor of going back to make a new copy from the original, preserving its integrity. But imagine that the copying isn’t done by a mindless scribe, but by someone trying to preserve intelligible words. They may turn a nonsense typo into a word but not necessarily the original, as in the childhood game of telephone, where the initial sentence can be completely transformed as it makes its way around the circle. Changes that are selected in this way could yield a significantly different work.
Mutant viruses occur all the time as they replicate but usually fail to significantly affect function. As more and more mutations are added they may destroy the virus completely, as with a badly garbled manuscript. But given enough opportunity, with new words selected as in the game of telephone, new functions may emerge. When we see the same changes emerging many times, independently, that suggests the emergence of newer and possibly more virulent viruses. This is what we are seeing in the UK with variant B.1.1.7, the South African B.1.351, and elsewhere.
Are you concerned about the U.K. and South Africa variants, in particular?
Think about it this way: How many SARS-CoV-2 variants are there in the world? A single person infected with COVID-19 may produce more than 100 billion viruses—a million in just in one drop of saliva. It’s possible that a billion people are infected worldwide (more than 100 million cases have been diagnosed). If we made that many copies of Hamlet, we could count on the fact that every single possible typographical error in typing Hamlet will have been made by someone, somewhere. The more viruses there are out there circulating, the more chances there are for mutations that make a virus more dangerous. The best way to prevent the development of new or worse variants is to suppress the infection with smart public health measures like masking and distancing, and vaccines.
How effective are the approved vaccines from Moderna, Pfizer, and Johnson & Johnson against these newer variants?
There are a couple of really important points to keep in mind. First, how effective a vaccine is depends on the question you ask. Is it 90 percent effective in preventing you from ever getting infected? Or 90 percent effective in preventing you from getting sick? Or 90 percent effective at preventing hospitalization or death? These are different endpoints. My understanding is that insofar as we can tell, all of the current vaccines are still very effective at preventing serious illness and death, even from these new variants. The data available to date is that the response to (and efficacy of) all these vaccines—against all viruses, in all populations—is excellent. They are far more notable for their similarities than their differences. If I were living in South Africa right now and had access to one of these vaccines, I would absolutely take it. I might still get sick, but I'm less likely to die.
A second point to keep in mind is that because of the way these vaccines have been constructed, reengineering them to recognize the variants will probably be relatively easy. The variant viruses we are now seeing are nowhere near as different as an influenza virus from one season to the next and we create flu shots every year. If a modified SARS-CoV2 vaccine that handles these variants is needed, it would probably take just a few days to create, and a few months to scale up for distribution.
Do you think COVID will require a new vaccination every year like the flu?
Many of us are asking, what's the future of this virus? Does COVID-19 go away completely and never come back, which is apparently what occurred with the original SARS virus? Will it stay with us like the other common human coronaviruses that are one of the causes of the common cold? If it stays with us, is it as innocuous as a cold virus—perhaps because adults are now immune, and children don’t develop severe disease—or will continued vaccination be required? If an ongoing vaccination program is required, will the vaccine protect us for life (as with the measles vaccine), or will annual vaccination be required to cope with new variants (as for influenza)? I don't have a crystal ball, but my guess is it will probably persist as a serious human cold virus for which vaccination is advisable. There are many reasons to suspect that this virus will not change as dramatically from year to year, so I am optimistic that annual revaccination will not be necessary.
Is the COVID-19 pandemic a once-in-a-lifetime experience, or is an outbreak like this something we might face again?
If we look back over history and try to project forward, it would not shock me to have to go through this experience again in my lifetime. There are many reasons for this, including the encroachment of human populations on the natural world. It's no surprise that Ebola, SARS, MERS, COVID, and HIV have all emerged from reservoirs in animal populations. There is every reason to think that something like this could happen again, but there is also much that we can do to minimize this risk, and to recognize and control new infections as they emerge.
What do you predict this summer looks likes for Americans? Would you book a vacation for August?
I'm hopeful, but there are too many unknowns at present to predict with confidence. If everyone in the world were to seriously lock down for the next month there's no question that we could travel in August, but that's not realistic, so a lot depends on the scale-up, effective distribution, and public acceptance of vaccines, including new vaccines not yet on the market.
Personally, having carefully read all of the public documents filed with the FDA and other agencies around the world, I have high confidence in all of the approved vaccines, I will show up for vaccination—with whichever vaccine is available to me—as soon as I’m eligible. I’ll also continue to follow common-sense public health measures, like wearing a mask even after being vaccinated, at least until we know that vaccination prevents not just the high level of infection that makes people sick, but even lower levels that might be transmissible. I hope that we can all follow public health measures until we flatten the curve down to nothing.