Pain Management
Jessica Wojick, doctoral candidate in the Department of Biology, examines the inner workings of chronic pain, and how to mitigate the suffering of those who are afflicted.
“How many of you have ever stepped on a Lego?” Jessica Wojick asked a crowd at a recent lecture. Two follow-up questions: Did you recoil at the thought of that? Or re-live the “ouch” moment in your head? If you did, “that’s because pain is complicated,” says Wojick, a doctoral candidate in the Department of Biology. It can feel like a mortal enemy and can also serve as protector.
But what governs pain? What processes do the body and mind undergo when they experience—and cope—with it?
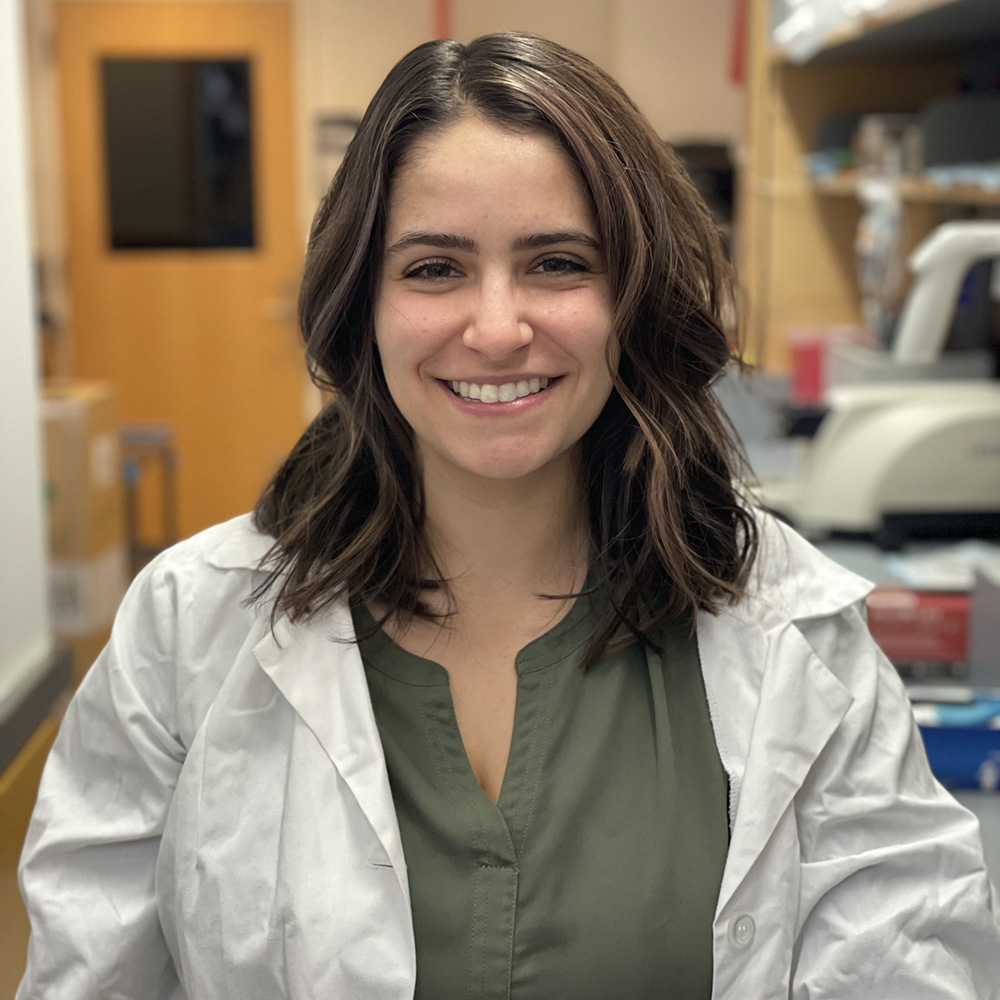
Jessica Wojick is a doctoral candidate in the lab of Penn Medicine’s Gregory Corder, an assistant professor of psychiatry. (Image: Courtesy Jessica Wojick)
“If you touch a hot stove, it will activate specialized neurons in the peripheral nervous system called nociceptors, and those nociceptors will send a signal to your spinal cord, which will then eventually send a signal to the brain,” says Wojick. “Even with something as simple as sitting in one position in your chair for too long, nociceptors can become activated, which unconsciously tells you to shift your body to avoid putting too much pressure on a particular joint. This is how we learn about our environment, like what to avoid, and it also allows us to learn to rest and recover when we do have an injury.”
Wojick breaks down the experience of pain into three component stages: sensory, cognitive, and emotional. The sensory component derives from the physiological response—the pinching sting of a bee, for instance—while the cognitive aspect is how the brain reasons through the trauma and how to potentially avoid it in the future. Finally, there is the emotional component: This hurts. How do I deal with it moving forward?
That third stage, the emotional component, is where Wojick’s research enters the picture, as she tries to understand how we might allay the suffering of people experiencing chronic pain.
A Personal Journey
Wojick was fascinated by the sciences early on and initially coupled this with a love of animals. She started down the veterinary track during her undergraduate studies at the University of Pittsburgh, and while she felt right at home working with the animals, it was the underlying research that lit a fire in her. Subsequent neuroscience classes and independent research pushed a fascination with the behavioral sciences to the fore.
When it comes to conquering pain in a controlled manner that doesn’t interfere with the body’s protective instincts, what has Wojick found to be one of the most promising solutions? Light, it turns out.
When Wojick eventually landed at Penn for her doctoral studies, she researched opioid use disorder and depression in the lab of Julie Blendy, a professor of pharmacology in the Perelman School of Medicine, before transitioning to Professor of Biology Marc Schmidt’s lab, where she studied the neurobiology and mating behavior of songbirds. Wojick then discovered an appointment in the lab of Penn Medicine’s Gregory Corder, an assistant professor of psychiatry, which seemed to combine all her previous interests—and touched upon her own personal experience, too.
“The lab, which focused on the neurobiology of pain, had just opened, and I became really interested in that, particularly because I suffer with chronic pain myself, as does one in five people,” says Wojick. “Also, around that same time, my grandmother was at the end of her journey with cancer, and she was really struggling with chronic pain. And so it just became very apparent to me that the medications that we had currently were not sufficient to help people in severe pain.”
Tracking Pain’s Neurological Origins
Though the majority of Wojick’s research is done using mouse models, she sees potential down the line for interventions that could aid people in chronic pain, like her grandmother was. The research itself centers on a specific region in the brain closely associated with the emotional stage of pain: the amygdala.
This association was famously highlighted in a procedure performed in the mid-20th century on a patient named Henry Molaison—best known as H.M.—who underwent a temporal lobectomy to combat severe seizures. Afterwards, Molaison presented a deficiency in his emotional pain response when heated probes were tested on his skin: He did not describe any as painful, no matter how hot they were.
Wojick is trying to understand what happens in situations like with Molaison, as well as what occurs in the brain in positive or rewarding situations, such as imbibing a sweet drink. “When neurons are active, they fire action potentials, and this involves a change in the electrical potential of the cell,” says Wojick. “When this firing occurs, there’s a big influx of calcium into the cell. Through the use of a tool that can detect this calcium using fluorescence, we can get a sense for how active the cells are.”
To do this, Wojick records what’s going on in these cells, monitoring the axon—a portion of the neuron—activity from the amygdala to another brain region called the nucleus accumbens. This provides a better understanding of how the activity of these cells changes in acute and chronic pain and informs how to potentially apply techniques that mitigate such pain.
An “On/Off” Switch for Pain
When it comes to conquering pain in a controlled manner that doesn’t interfere with the body’s protective instincts, what has Wojick found to be one of the most promising solutions? Light, it turns out. Specifically, a technique called optogenetics that acts as a sort of “protein light switch,” says Wojick. Derived from algae, these genetic proteins turn off the active “pain” cells when light is shone on them.
The introduction of this light can effectively shut off the emotional response to pain—the “ouch” response—without doing the same to the sensory component, which is important in teaching us what is and isn’t safe for our bodies, she explains. Though humans can modulate pain to an extent—for example, when voluntarily undergoing acupuncture, tattooing, or, as Wojick highlights, a performer walking on a bed of nails—pain is still foundationally critical to human existence, acting as an instinctual learning mechanism for dangers to avoid.
Rare cases of genetic mutations have shown that those incapable of experiencing pain can be in constant danger of injury, because they lack this sensory response. This is something that occurs even in patients like Molaison, who react to pain with reflex, even though pain’s unpleasantness isn’t “felt.” Optogenetics and other promising drugs and therapies that target cells in the amygdala remove the emotional component, leaving alone the body’s natural sensory response. The hope is that the techniques will continue to advance, providing customized pain treatment for those with chronic symptoms.
Looking to the future, Wojick says these techniques also have the potential to treat complex conditions. “Currently, there are some patients who use deep electrical brain stimulation,” she says. “They already have implants that stimulate dopamine neurons in their brain, but it would be beneficial if we could develop less invasive techniques to target brain cells that show pathological activity, whether in diseases like Parkinson’s or in chronic pain disorders.”