Cancer Cells Selectively Use ‘Drones’ to Keep T Cells From Infiltrating Tumors
Wei Guo, Class of 1965 Term Professor of Biology, identifies a new tool to help predict how a patient might respond to checkpoint inhibitor drugs.
Checkpoint inhibitor drugs have been a gamechanger for many cancer patients. Yet around 70 percent don’t respond to these medications, which work by removing the “brakes” on the immune system’s response to a tumor. In some non-responders, the immune system’s killer T cells can’t penetrate the tumor boundaries.
In a new study, Wei Guo, Class of 1965 Term Professor of Biology, identified a mechanism responsible for keeping killer T cells from infiltrating a tumor. The work, published in Nature Communications, offers a new tool to predict how a patient might respond to checkpoint inhibitor drugs.
“Infiltration of the tumor is crucial for the success of checkpoint blockade therapy,” says Guo, senior author on the work. “Because this T cell infiltration is so crucial, it’s also important to know the molecular mechanism of how it works and when it doesn’t.”
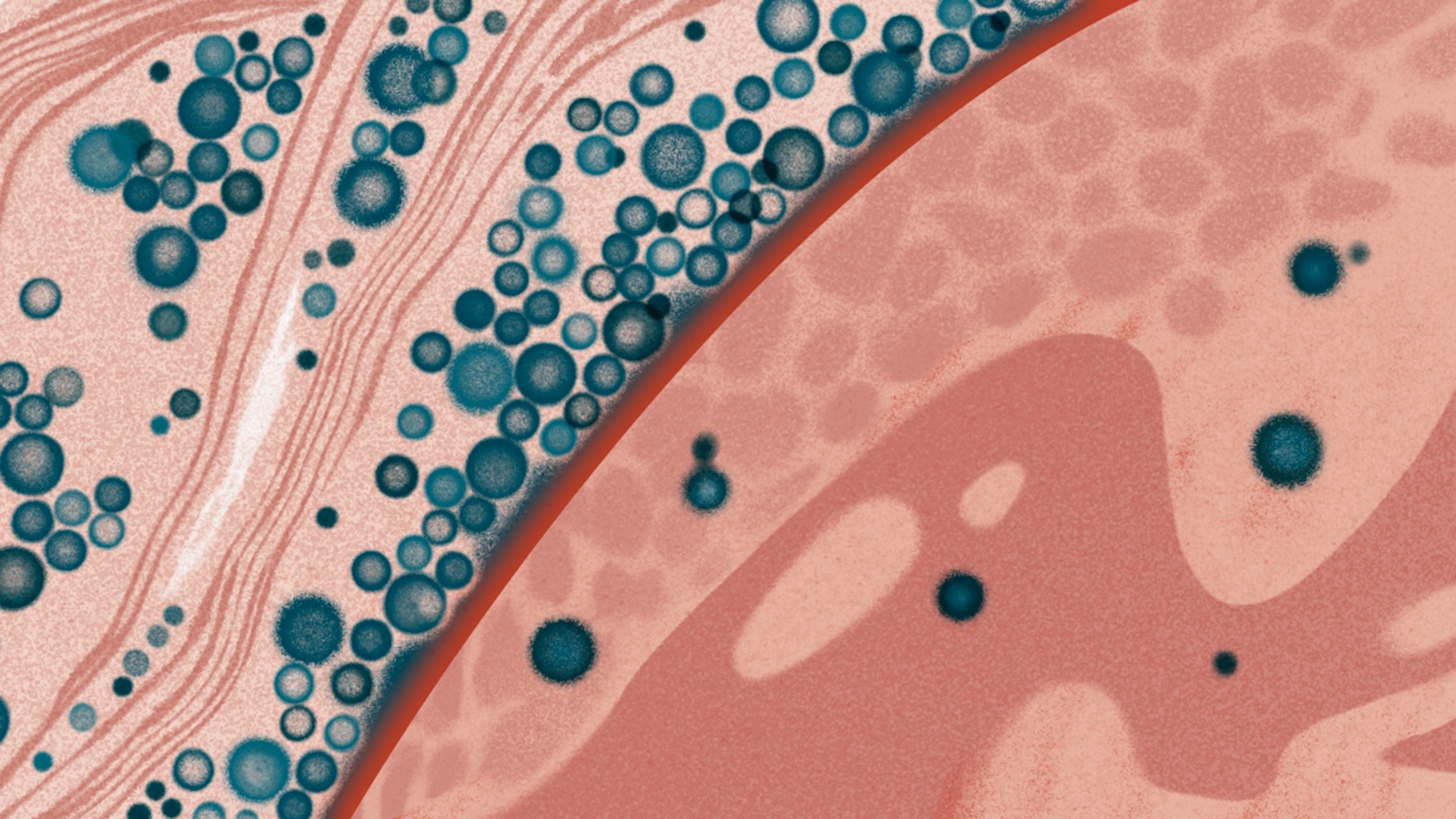
Guo’s lab has explored how cancerous tumors secrete exosomes, small vesicles that serve as biological drones that do battle with the immune system at sites well away from the primary tumor. Exosomes loaded with the protein PD-L1 can interact with T cells’ PD-1 protein, causing the T cells to tire before they reach the tumor. “If you consider exosomes as drones, then PD-L1 is the weapon loaded on the drone,” Guo says.
Many checkpoint inhibitor drugs block this interaction, aiming to keep T cells invigorated and ready for a fight. Guo and colleagues wanted to understand how cancer cells load their “drones” with PD-L1, and whether this activity prevents T cells from infiltrating tumors.
Turning their focus to the process by which cancer cells generate exosomes, the researchers paid particular attention to a molecule called HRS, a member of a large complex called ESCRT involved in sorting the “cargo” placed in exosomes. In the lab, they looked in metastatic melanoma cells and found that frequently ERK, an enzyme well known to be activated in melanomas, added a phosphate group to HRS.
“We hypothesized that the tumor is regulating HRS, which has a major role in generating exosomes and uploading PD-L1 to their exosomes,” Guo says.
Guo and colleagues created different cancer cell lines, some of which had regular HRS, and some of which had HRS with either reduced or elevated levels of phosphorylation. Mice exposed to the more highly phosphorylated HRS developed tumors that grew significantly faster; these animals also had lower levels of T cell infiltration in their tumors.
When the researchers gave these mice a checkpoint inhibitor drug that blocked PD-1, the tumors did not respond. Yet when they added an ERK inhibitor drug, the tumors shrank. Further studies showed that exosomes processed by phosphorylated HRS had cargos enriched with PD-L1, promoting resistance to the checkpoint blockade.
In tissue samples from melanoma patients, different areas of the tumors had varying levels of phosphorylated HRS. “In the areas of the tumor with a lot of phosphorylation, the T cells stayed outside the border,” says Guo. “They just could not cross.”
The findings suggest that screening cancer patients’ tumors for HRS phosphorylation may help predict their responsiveness to checkpoint inhibitors. And reducing HRS phosphorylation could be a strategy for boosting the immune system’s defenses against cancer. While ERK inhibitors alone could be toxic, says Guo, an approach that blocked phosphorylation of HRS specifically could prevent it from loading PD-L1 to exosomes in the first place.
Guo’s group will continue investigating how tumor cells can be so selective in choosing which cargo to send out in exosomes—and how T cells, in turn, can selectively send out their own exosomes to fight back.
“It’s a clash of two titans,” Guo says.



